Three critical considerations for provider collaboratives in Health and Social Care

key fact
Provider collaboratives can reduce care variability, enhance resource efficiency, and improve patient outcomes through shared decision-making and integrated services.
Paul Fountain-Edgar explores three key questions to consider when transforming to provider collaboratives for Integrated Care Services. In what is currently an uncertain environment, he says, tackling the trickiest strategic headlines now will guard against the change roadmap veering off course down the line.
Ambitions to transform health and social care at scale are nothing new. Moving to an integrated model of care (a core directive of the Health and Care Act 2022) is firmly at the heart of the sector’s change agenda. But a new UK government, Lord Darzi’s recent review of the NHS, and the government’s initial response, bring even more urgency to the landscape. Three major change initiatives are on the table according to our new Health Secretary: the shift from hospital to community-led care, from analogue to digital, and (perhaps most importantly to safeguard the NHS’s long-term future), from reactive treatment to preventative care.
All of these, of course, will be fundamentally enabled by technology change across the entire health and social care ecosystem, from point of care applications through to patient-facing solutions and back-end services. Especially when it comes to the latter, the move to provider collaboratives sees technology leaders walking a transformation tightrope. Balancing collaboration, optimisation, and cost efficiencies with the need to build the foundations for the future of integrated care is a complex business. Doing it in the context of stubborn technical debt, cultural siloes and critical financial deficits is even more difficult. Now, as we wait for further detailed directives to support the government’s headline ambitions, we must add a likely degree of uncertainty into the mix.
As the NHS guidance confirms, systems and their constituent providers have flexibility to decide how best to arrange provider collaboratives, although flexibility does not mean complete autonomy and there are frameworks in place to guide the process. In corporate services, a number of delivery models are available:
Figure 1 – Shared capability delivery models
The flexibility is welcome, since it allows those on the transformation frontline to adapt their strategy to the particular Integrated Care Board (ICB)’s environment, stakeholders, objectives and challenges. We see examples of this in ICBs across the UK, each implementing their own iterations of these delivery models. Across all of them, the core theme is technology standardisation, with all of the efficiencies and benefits that brings. From our own experience of supporting transformation in health and social care, there are three core considerations that must be addressed right from the start to prevent unnecessary risks creeping in – now, or (even more worryingly) at some indeterminate point down the line. Because, by that time, it will be far too late to turn the ship around.
Aligning the governance structure to the delivery model
First, serious consideration should be given to how governance will operate, and how that will impact on the ability to deliver. The committee in common, for example, might seem the most flexible approach. It allows us to leverage the benefits of local ‘best in breed’ expertise and gives all stakeholders a voice at the table across all leadership decisions. But, as we wait for further government guidance on both policy and funding that may well demand significant change, the most effective thing that we can do as technology professionals is to be ready to pivot if and when that change comes. Decisions will need to be made – and quickly. With no central autonomy, the committee in common risks roadblocks if different organisations and stakeholders cannot agree.
On the other hand, a joint committee structure allows less scope for widespread input on every decision, but it does incorporate leadership representation from each organisation while also facilitating centralised decision-making and – importantly – increased funding certainty. While the structure seems more rigid, it may actually allow for more agility by entrusting the nominated leadership to respond – rapidly and decisively – to unpredictable factors, while keeping a firm eye on the central objectives. In this kind of major transformation programme, with so many complex interdependencies, ensuring that the governance structure is right, right from the start, is no easy business in itself.
Building the right culture to support the ongoing change
By necessity, moving to provider collaboratives means combining and rationalising multiple functions across multiple organisations. That involves serious change – and change, by its nature, is scary. From your people’s perspective, this is about more than simply swapping their organisational T-shirt on a particular nominated day. They need to understand and be part of the ongoing change journey without feeling threatened by it. Because, in the midst of a major transformation, the last thing you need is to lose valuable talent and the rich repository of knowledge that people bring to their roles.
This area demands careful cultural management. By and large, ‘big bang’ approaches to rolling out transformation initiatives should be avoided from a people perspective. A careful, iterative roadmap of continuous improvement and incremental consolidation strikes a better balance. It takes the transformation in the direction it needs to go to achieve the ultimate outcomes, while avoiding possible panic, rumour and resentment amongst staff. The key consideration here is mapping where, and how, opportunities for change and rationalisation will logically arise, and being ready to leverage them at the right time. That is no small undertaking, but it should be a part of planning the journey, from the outset.
Planning the process of delivering the change
Both of the above are critical considerations, but the area that arguably carries the most risk of creep, cost and failure is the delivery process itself. In my experience, the key here is to design the delivery journey so that it takes full account of the multiple, complex factors that will influence success.
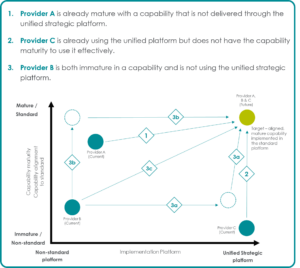
Figure 2 – Platform-driven capability convergence
In fact, this doesn’t have to be a case of selecting one approach at the expense of any other. Multiple factors and interdependencies will come into play. Maturity and capability levels across the different involved organisations, speed to delivery, risk, cost, and legacy ways of working (to name just a few considerations) will all affect how any Integrated Care Board builds its delivery journey. Not to mention anticipating and building in future technology considerations. The move to preventative care, in particular, will depend heavily on leveraging AI, automation, and data integration and management. Does a ‘tool sooner’ approach risk investing heavily now in technology that may not be geared up to support those evolving capabilities? If not, what might seem like a quick win on the transformation roadmap now could quickly turn into another technical debt issue in three to five years’ time, with all of the expense, complexity and headaches that will inevitably bring.
All of these considerations are deeply challenging to unravel! Daunting though the landscape might be, we should embrace it. As technology and IT professionals, we have a key opportunity here to make a profound impact on the future of health and social care in the UK, by transforming the technology services and delivery that will ultimately underpin the health and social care models of tomorrow.
Paul Fountain-Edgar is Mason Advisory’s Head of Health and Social Care. If you would like to explore these issues – or any aspect of the sector’s change and transformation challenges – simply contact us at health@masonadvisory.com to book an appointment.
Plus, you can explore our work in the Health and Social care sector here, or explore our IT change services portfolio here.